COBRA Administration – How we help you
by Paul Devlin
Many employers still do not fully understand what they are required to do with COBRA. Working with APlus, you will not only minimize your liability associated with administering the program, but save yourself countless hours of work. Proper COBRA compliance entails many required notices and tracking numerous time frames. The notice requirements and the work related to them are endless.
With APlus you can spend your time managing your workforce, not administering COBRA and the timeframes and notices that go with it. With Certified COBRA Administrators on staff and state-of-the-art technology, we ensure COBRA, Open Enrollment, State Continuation, USERRA and Eligibility are all handled properly.
Most administrators require you to enter new plan member and qualified beneficiary information into their system through the employer portal, but because we have access to your employee and benefit information in the UKG Ready system, you have the option to let us enter it for you, saving you time. Either way, we can configure reports and notifications to help get member information entered in the COBRA system.
How to Streamline your workflow using our technology
Save time, reduce manual processing, and stay in compliance.
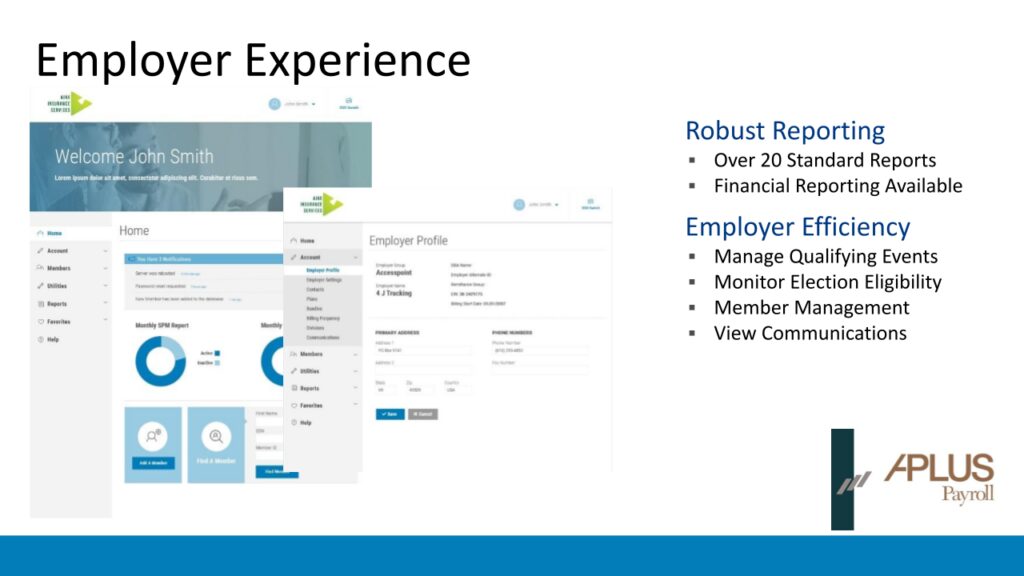
From financial reporting for tracking premium disbursements and settlements, automatically monitoring terminations and elections, 834 file transformation and mapping, to managing employee questions and issues, you can do it all (and view real-time updates) in the COBRA employer portal.
Access robust, on-demand reporting.
No more waiting for reports! Employers can quickly run reports on-demand in a variety of formats and/or take advantage of custom reporting solutions.
Customize the participant experience.
Extend your brand and style through colors, your logo, fonts, and via letters so your participants know they are working with you.
Drive efficiency with integrations.
You save time (and money) when leveraging our integrations.
View real-time data.
With us, you get complete transparency with access to all communications and reporting in real-time.
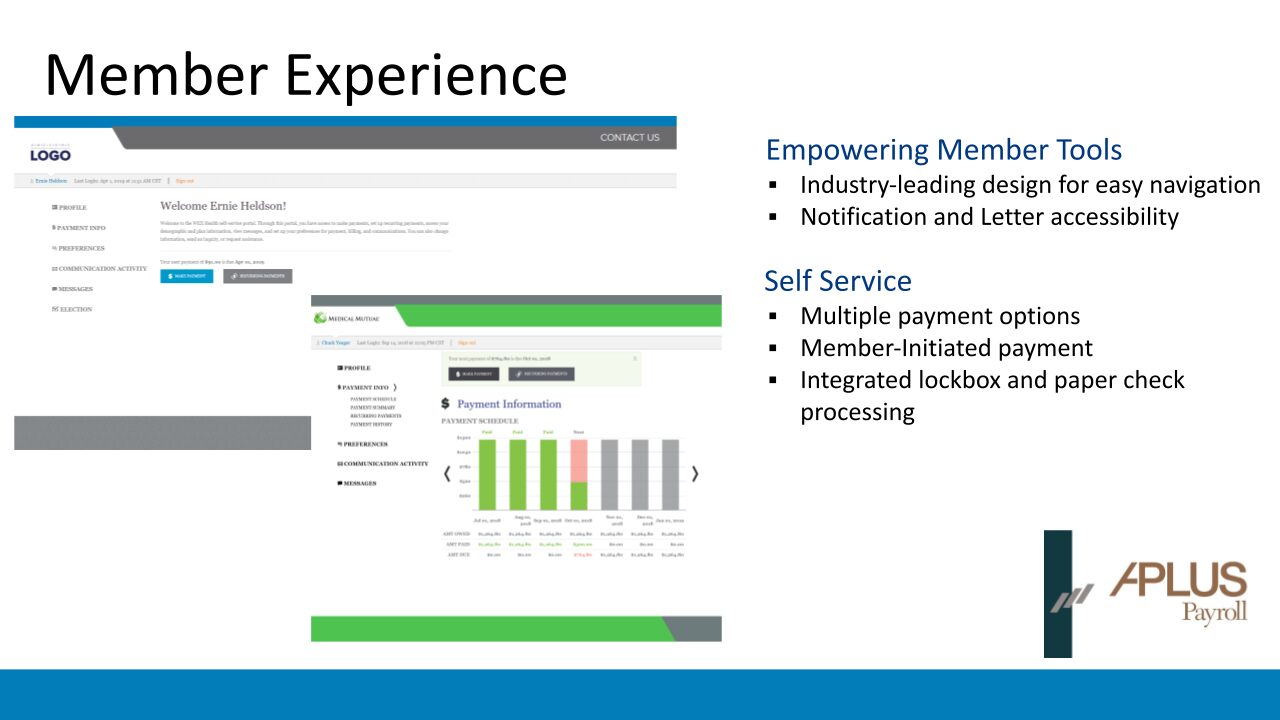
Access their account information online.
Our intuitive platform makes it easy for participants to make elections, submit payments, view their statuses, make open enrollment elections, and get help when they need it (24/7).
Stay connected via mobile app.
Nearly everyone has a smartphone (even if they don’t have a computer), which means that participants can maintain access to their COBRA and direct bill account when they leave your company (or are simply on-the-go).
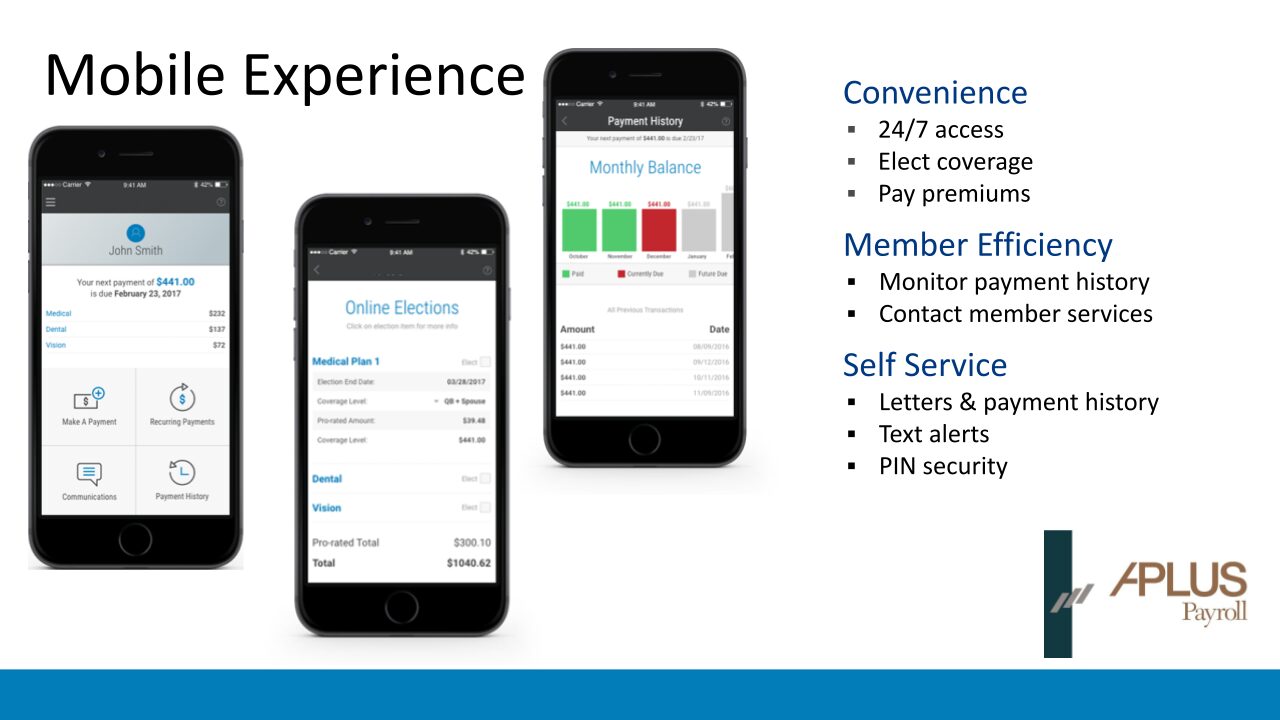
View real-time payments.
Some systems take days to update after a participant makes a payment (which increases call volumes). But with us, participants get real-time, immediate updates to their account after making a payment.
Make open enrollment elections online.
When life changes, oftentimes benefits need to change, too. COBRA and direct bill participants can make open enrollment elections online and choose different plans, add or drop dependents, and more.
Receive automated, clear communications.
Our COBRA and direct bill letters are editable and separate (so you can make sure every letter is clear to avoid confusing calls from participants). Plus, letters and notifications are fully automated to save time and stay in compliance.
More than software
We offer integrated services, such as payment processing and mail fulfillment, to reduce processing errors and keep you compliant.
Payment processing
Billing/payment processing integrated into one system.
Mail fulfillment
Fully automated and compliant solution that is highly scalable (which makes it easy to manage erratic volume), and is completely hands-off with bar code technology.